ME- en multisystemisk sygdom
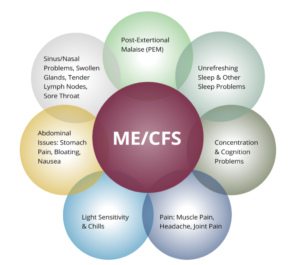
Der er international konsensus for, at ME er en multisystemisk sygdom, hvor flere af kroppens systemer angribes samtidigt, hvilket ligger i tråd med patienternes symptomer. På denne side finder du et kort udpluk med link til de seneste års forskningsresultater inden for de organsystemer, som ME angriber. Det viser bredden af denne multisystemiske sygdom. Der vil også være artikler fra den faste forskningsklumme i ME nyt, ME Foreningens medlemsblad. Overordnet er der ofte tale om autonom dysfunktion.
Danish Medical Journal publicerede i 2022 en artikel om emnet.
ME Forskningsoversigt
Læs Foreningens Videnskabsfolder 2023 der giver en videnskabelig oversigt over ME-forskningen.
Derudover brinner denne side links til den hastigt voksende biomedicinske ME-forskning. Artiklerne er ordnet efter emne, dvs, med reference til sygdomsmekanismer i ME. De mest fremtrædende teorier, refererer henholdsvis til:
- immunforsvaret (autoimmunitet, immundefekt, eller kronisk infektion),
- mavetarm-systemet, nervesystemet (herunder hjernen)
- mitokondrierne (metabolismen)
- genetikken
Bemærk at man inden for forskningen bruger betegnelsen ME/CFS. Så i forskerverdenen skal man ofte betragte de to betegnelser som synonymer.
1. Immunforsvaret, autoimmunitet, immundefekt, kronisk inflammation
- Loebel, Fluge, Mella et.al. 2015): Antibodies to ß adrenergic and muscarinic cholinergic receptors in patients with Chronic Fatigue Syndrome. Antistoffer mod Beta- og M-nervereceptorer hos patienter med CFS.
- Morris, Maes (2013):The Emerging Role of Autoimmunity in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. (Den fremspirende rolle, som autoimmunitet har fået hos sygdommen ME/CFS). Tidsskriftet Molecular Neurobiology).
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome – Evidence for an autoimmune disease
Immundefekt
- Nguyen et.al. (2017). Impaired calcium mobilization in natural killer cells from chronic fatigue syndrome/myalgic encephalomyelitis patients is associated with transient receptor potential melastatin 3 ion channels. (Nedsat calciummobilisering af de naturlige dræberceller hos CFS/ME-patienter bliver sat i forbindelse med TRPM3 ion-kanalen).
- Hornig, Montoya, Peterson, Komaroff, Lipkin et.al. (2015) Distinct plasma immune signatures in ME/CFS are present early in the course of illness. (Bestemte immunsignaturer i blodplasma viser sig tidligt i sygdomsforløbet).
- Multiple co-infections (Mycoplasma, Chlamydia, human herpes virus-6) in blood of chronic fatigue syndrome patients: association with signs and symptoms, Nicolson, et al.APMIS. 2003 May;111(5):557-66. http://www.ncbi.nlm.nih.gov/sites/entrez
- Activation of human herpesviruses 6 and 7 in patients with chronic fatigue syndrome,Chapenko et al.J Clin Virol. 2006 Dec;37 Suppl 1:S47-51
- http://www.ncbi.nlm.nih.gov/pubmed/17276369
- https://www.docdroid.net/xqMXUb8/me-gr-att-bota.rtf.html
- http://www.ncbi.nlm.nih.gov/pubmed/15642984
Infektion/Neuroinflammation
- https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8721200/?s=09
- Chronic viral infections in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)(2018)
- Underhill (2015): Myalgic encephalomyelitis, chronic fatigue syndrome: An infectious disease (ME/CFS: en infektionssygdom)
- (2009): Chronic Fatigue Syndrome After Infectious Mononucleosis in Adolescents (CFS efter mononucleose-infektion hos unge)
- Chia & Chia (2008): Chronic fatigue syndrome is associated with chronic enterovirus infection of the stomach (Kronisk træthedssyndromer forbundet med kronisk enterovirusinfektion (virussmitte overført via afføring i maven)).
- http://www.ncbi.nlm.nih.gov/sites/entrez
- http://www.ncbi.nlm.nih.gov/pubmed/17276369
- http://www.ncbi.nlm.nih.gov/pubmed/19414405
- http://jcp.bmj.com/cgi/content/abstract/61/1/43
- https://pubmed.ncbi.nlm.nih.gov/35832182/
2. Mave-tarmsystemet, Nervesystemet (herunder hjernen)
- Sorenson et.al.(2014): Brain Derived Neurotrophic Factor is Decreased in Chronic Fatigue Syndrome and Multiple Sclerosis. (Hjerneafledt neurotrofisk faktor er reduceret ved CFS og multipel sklerose).
- Komaroff et.al. (2011): EEG spectral coherence data distinguish chronic fatigue syndrome patients from healthy controls and depressed patients-A case control study. (EEG-hjerneskanning kan skelne CFS-patienter fra sunde kontrolpersoner).
- Shukla, Frank, et.al. (2015): Changes i Gut and Plasma Microbiome following Exercise Challenge in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. (forandringer i mave- tarmfloraen som følge af motion ved ME/CFS)
- Sanjay K. Shukla et al.The association of fecal microbiota and fecal, blood serum and urine metabolites in myalgic encephalomyelitis/chronic fatigue syndrome
- http://www.ncbi.nlm.nih.gov/pubmed/15642984
- http://www.ncbi.nlm.nih.gov/pubmed/19112401
- http://www.ncbi.nlm.nih.gov/pubmed/15955487
- Gray matter volume reduction in the chronic fatigue syndrome,
- http://www.ncbi.nlm.nih.gov/pubmed/12800454
- http://www.ncbi.nlm.nih.gov/pubmed/8542261
3. Mitokondriel dysfunktion
- ME og blodet
Forskerhold fra forskellige forskningsuniversiteter har publiceret en lang række artikler om ME-patienters blod, som adskiller sig på en række punkter fra raskes. - Fluge, Mella, Bruland et.al (2016): Metabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome. (Stofskifte-profilering viser nedsat mitokondrie-funktion som følge af enzymet PHD hos ME/CFS-patienter).
- Brewer et al. (2013): Detection of Mycotoxins in Patients with Chronic Fatigue Syndrom (fund af mytotoksiner – svampegift hos patienter med CFS)
- Myhill et.al. (2013): Targeting mitochondrial dysfunction in the treatment of ME/CFS (Lindring af mitokondriel dysfunktion ved behandlingen af ME/CFS).
- Myhill et.al. (2009): Chronic fatigue syndrome and mitochondrial dysfunction (ME/CSF og mitokondriel dysfunktion).
- http://www.ncbi.nlm.nih.gov/pubmed/15796202
- Dysfunktioner i metabolismen hos ME patienter
PEM (Post excertional malaise)
- http://me-foreningen.dk/wp-content/uploads/2018/06/emerge.org_.au-Post-Exertional-Malaise-Exercise-And-MECFS.pdf
- https://academic.oup.com/ptj/article/93/11/1484/2735315/Discriminative-Validity-of-Metabolic-and-Workload
- https://www.researchgate.net/publication/41121299_Postexertional_Malaise_in_Women_with_Chronic_Fatigue_Syndromeemerge.org.au-Post-Exertional Malaise Exercise And MECFS
- http://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0145453#sec011
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4004422
- https://www.ncbi.nlm.nih.gov/pubmed/20937116
- https://www.ncbi.nlm.nih.gov/pubmed/16260962
- https://www.ncbi.nlm.nih.gov/pubmed/20095909
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2757484/
- https://www.ncbi.nlm.nih.gov/pubmed/21615807
- https://www.ncbi.nlm.nih.gov/pubmed/20230500
- http://www.ncbi.nlm.nih.gov/pubmed/20469961
- Light AR, Bateman L, Jo D, Hughen RW, Vanhaitsma TA, White AT, Light KC. Gene expression alterations at baseline and following moderate exercise in patients with Chronic Fatigue Syndrome, and Fibromyalgia Syndrome. J Intern Med 2012; 271: 64-81. [PMID: 21615807]
- https://www.ncbi.nlm.nih.gov/pubmed/20038921
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3022475/
- https://www.ncbi.nlm.nih.gov/pubmed/20038921
- https://www.ncbi.nlm.nih.gov/pubmed/18942064
- http://www.ncbi.nlm.nih.gov/pubmed/15715687
- http://www.ncbi.nlm.nih.gov/pubmed/11088089
- http://www.ncbi.nlm.nih.gov/pubmed/15790422
- http://www.ncbi.nlm.nih.gov/pubmed/11528333
- http://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0145453#sec011
4. ME og Genetik
Oversigt over de gener man i forskningen har fundet påvirkede hos ME patienter
- https://www.ncbi.nlm.nih.gov/pubmed/16610957
- https://www.nature.com/articles/tp2015208
- http://www.clinexprheumatol.org/article.asp?a=2817
- http://jcp.bmj.com/content/jclinpath/58/8/860.full.pdf
- https://www.ncbi.nlm.nih.gov/pubmed?Db=pubmed&Cmd=ShowDetailView&TermToSearch=27834303
- https://www.ncbi.nlm.nih.gov/pubmed?Db=pubmed&Cmd=ShowDetailView&TermToSearch=27099524
- https://www.ncbi.nlm.nih.gov/pubmed?Db=pubmed&Cmd=ShowDetailView&TermToSearch=27835969
- https://www.ncbi.nlm.nih.gov/pubmed?Db=pubmed&Cmd=ShowDetailView&TermToSearch=26272340
- https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-017-0248-3
- https://www.ncbi.nlm.nih.gov/pubmed?Db=pubmed&Cmd=ShowDetailView&TermToSearch=26230484
- http://www.ncbi.nlm.nih.gov/pubmed/18462164
- ME og gener
- Forskningsartikler i andre ME-symptomer
- 11 Fysiske fund i ME Oversigt over biomarkører Svensk Ugeskrift for lægerCardiac and circulatory problems“The patients with severe CFS had significantly lower stroke volume and cardiac output than the controls.”Abnormal impedance cardiography predicts symptom severity in chronic fatigue syndrome,Peckerman A et al. Am J of the Med Sciences, 2003; 326(2):55-60
http://www.ncbi.nlm.nih.gov/pubmed/12920435“A progressive cardiomyopathy caused by incomplete virus multiplication of EBV and/or HCMV in CFS patients is present.”Prevalence of abnormal cardiac wall motion in the cardiomyopathy associated with incomplete multiplication of Epstein-Barr Virus and/or cytomegalovirus in patients with chronic fatigue syndrome, Lerner et al. In Vivo. 2004 Jul –Aug;18(4):417-24
https://www.ncbi.nlm.nih.gov/pubmed/15369178 Cognitive problems
“Individuals with CFS appear to have to exert greater effort to process auditory information as effectively as demographically similar healthy adults.”Objective evidence of cognitive complaints in Chronic Fatigue Syndrome: A BOLD fMRI study of verbal working memory, Lange G et al. Neuroimage 2005 June; 26(2):513-24
http://www.ncbi.nlm.nih.gov/pubmed/15907308 Orthostatic intolerance
“Symptoms of orthostatic intolerance, such as disabling fatigue, dizziness, diminished concentration, tremulousness, and nausea, are often found in patients with CFS.”Postural orthostatic tachycardia syndrome is an under-recognized condition in chronic fatigue syndrome,Hoad A, Newton. J et al.2008 QJM 2008 101(12):961-965 https://www.ncbi.nlm.nih.gov/pubmed/18805903 Sleep abnormalities
“Higher levels of deep sleep and/or lower levels of light sleep have been reported in several all-night polysomnography studies in CFS patients.”Paradoxical Nrems Distribution in ”Pure” Chronic Fatigue Patients. A Comparison With Sleep Apnea-Hypopnea Patients and Healthy Control Subjects,Le Bon O et al. Journal of Chronic Fatigue Syndrome, vol.14,(2 ) Jan. 2008, pp.45-59“CFS patients had significant differences in polysomnographic findings from healthy controls and felt sleepier and more fatigued than controls after a night’s sleep.”Sleep structure and sleepiness in chronic fatigue syndrome with or without co-existing fibromyalgia,Togo F et al. Arthritis Research & Therapy2008;10(3):R56.
http://www.ncbi.nlm.nih.gov/pubmed/18474105

